Preliminary short-term results of ankle arthroplasty with the Taric® prosthesis
DOI:
https://doi.org/10.30795/jfootankle.2020.v14.1132Keywords:
Ankle, Osteoarthritis, Surgery, Arthroplasty, Replacement, AnkleAbstract
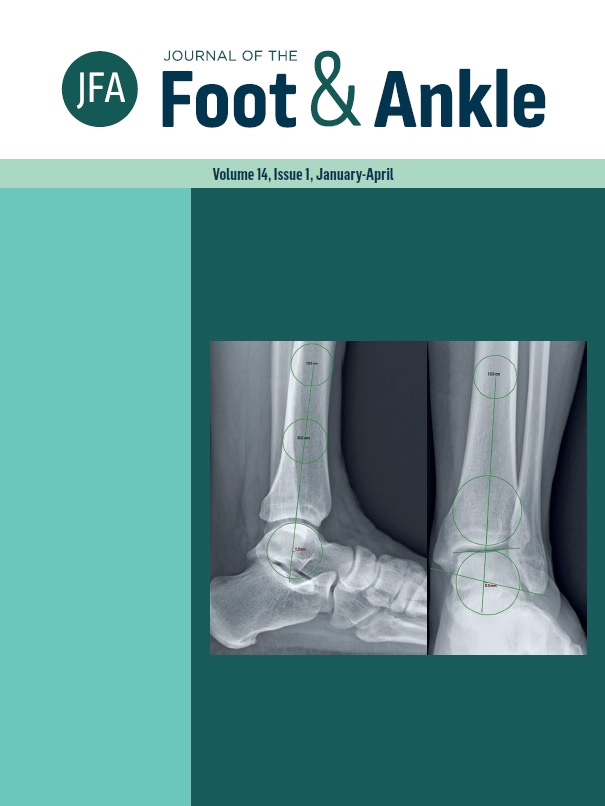
Objective: Present the clinical and functional outcome of the first five ankle arthroplasties performed in our department. Methods: Five patients (five feet) with secondary arthrosis of the ankle underwent ankle arthroplasty with the Taric® prosthesis. Average age at the time of surgery was 42 years. Follow-up time averaged 43 months. We recorded the immediate postoperative complications. For clinical evaluation we used the VAS pain scale, the AOFAS hindfoot and ankle scale, and the Foot Function Index. We measured the leg-foot range of motion. On the radiographs, we measured the alpha, beta, and gamma angles as well as sagittal balance. We sought to identify the presence of posterior osteophytes (bone spurs). Results: We observed a case of medial malleolus fracture and a case of superficial suture dehiscence. In two cases, we considered the final outcome to be poor. The mean VAS of pain before surgery was 8.8 points while the postoperative score was 5.4 points. On the AOFAS scale, the average preoperative score was 52 points and the score at final evaluation, 70 points. We noticed a 10º increase in leg-foot range of motion. Conclusion: The assessment of the first patients undergoing ankle arthroplasty with the Taric® prosthesis yielded outcomes considered poor in 40% of cases. However, in those with an outcome considered satisfactory, there was an improvement in pain and an increase in leg-foot range of motion. In all patients, we noticed the formation of a posterior osteophyte alongside the posterior cortex of the distal tibia. Level of Evidence IV; Therapeutic Studies; Case Series.