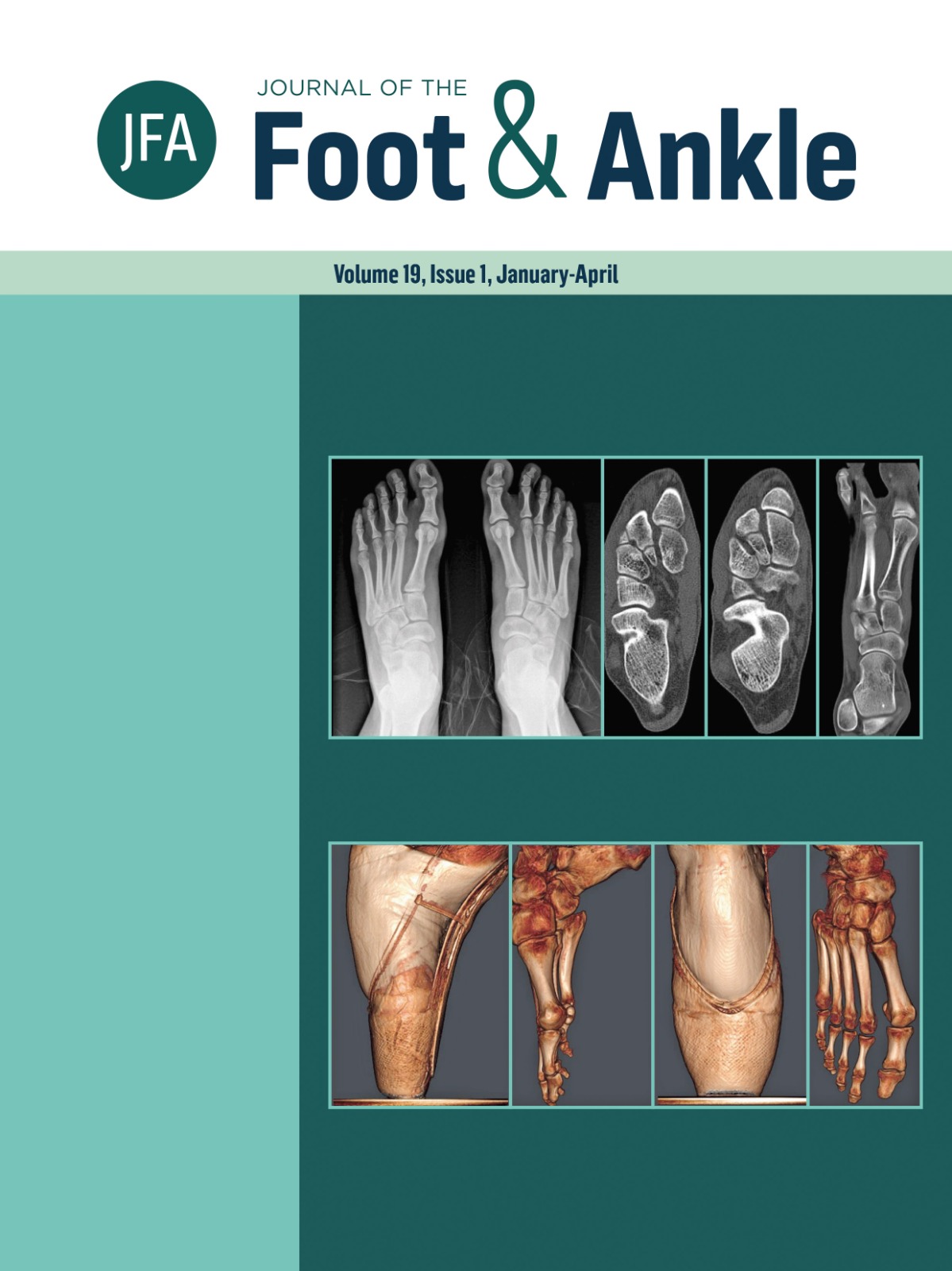
The role of subtalar arthroereisis in flatfoot treatment: insights from weight-bearing computed tomography
DOI:
https://doi.org/10.30795/jfootankle.2025.v19.1881Keywords:
Subtalar Joint; Flatfoot.Abstract
Flatfoot is a common deformity in adult and pediatric populations, with a 5% incidence. The three-dimensional deformity and the dynamic joint behavior during weight bearing are better understood with weight-bearing computed tomography (WBCT), making it an essential tool for diagnosis and staging. There is consensus about the indication for arthroereisis in symptomatic flexible flatfoot or hindfoot valgus in pediatric or adolescent populations; however, no studies to date have evaluated the degree of three-dimensional correction achieved in adult patients with progressive collapsing foot deformity (PCFD) treated with arthroereisis. A retrospective analysis of nine adult patients with symptomatic flexible flatfoot (15 feet) submitted to arthroereisis, was performed. WBCT before surgery and four months after the procedure were reviewed. Subtalar and talonavicular joint alignment was analyzed through specific measurements (Inftal-suptal, Inftal-hor, posterior facet subluxation, medial facet subluxation, calcaneal pitch, Meary’s angle, dorsal talar-1st metatarsal angle, and talonavicular angle). Inftal-hor, posterior facet subluxation, medial facet subluxation, Meary’s angle, dorsal talar-1st metatarsal angle, and talonavicular angle reached statistically significant differences. The talonavicular coverage angle showed a more considerable improvement with a mean of 33º in the preoperative vs 23º in the postoperative (p < 0.001). Calcaneal inclination (p = 0.195) and Ifthal-suptal (p = 0.656) had no statistical differences. Subtalar arthroereisis is an effective three dimensional correction procedure for adults with symptomatic progressive collapsing foot deformity. Level of evidence: V, Therapeutic studies - investigating the results of treatment; Expert opinion.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Journal of the Foot & Ankle

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.